Interpreting 12 Lead Ecgs Made Easy – One of the most useful and commonly used diagnostic tools is the electrocardiogram (EKG) which measures the heart’s electrical activity in waveforms. An electrocardiogram uses electrodes attached to the skin to detect the electrical current passing through the heart. These signals are transmitted to create a record of the heart’s activity. Arrhythmia is a disturbance of the heart’s normal rhythm caused by changes in the conduction of electrical impulses. These impulses stimulate and coordinate the contraction of the atrial and ventricular muscles to provide cardiac output.
Have you ever wondered how nurses and doctors can easily read the ECG card? How can they distinguish atrial tachycardia from atrial fibrillation, or do they know what atrial fibrillation or tachycardia is?
Interpreting 12 Lead Ecgs Made Easy

Interpreting an EKG requires great skill, a sharp eye and a good theoretical background in various arrhythmias as well as concepts about cardiac conduction and the EKG machine. EKG interpretation skills take time to develop, but once you get the hang of it, you’ll be able to interpret any squiggly line on EKG paper.
Amazon.com: Ekg Pocket Card: 9781941004067: Aprn World: Books
Causes of sinus tachycardia can include exercise, anxiety, fever, medications, anemia, heart failure, hypovolemia and shock. Sinus tachycardia is often asymptomatic. However, management is directed towards treating the underlying cause. Carotid sinus pressure (carotid massage) or beta blockers may be used to slow the heart rate.
Sinus bradycardia is a heart rate below 60 beats per minute and originates in the sinus node (as the word “sinus” refers to the sinus node). It has the following features
Causes may include drugs, vagal stimulation, hypoendocrine conditions, hypothermia, or sinus node involvement in MI. These arrhythmias can be common in athletes because they have a good heart rate. It is often asymptomatic but symptoms may include: fainting, fatigue, dizziness. Management consists of treating the underlying cause and using anticholinergic medications such as atropine sulfate as prescribed.
Atrial premature contractions are ectopic beats that originate in the atria and are not rhythmic. Heart cells start working or stop working before the heart has a normal rhythm. These are called tachycardia and have the following symptoms:
Ekg Interpretation Cheat Sheet & Heart Arrhythmias Guide (2020 Update)
Causes include coronary artery disease or valvular heart disease, arterial ischemia, coronary atherosclerosis, heart failure, COPD, electrolyte imbalance, and hypoxia. Treatment is usually not necessary but may include the use of procainamide and quinidine (antiarrhythmic drugs) and carotid sinus massage.
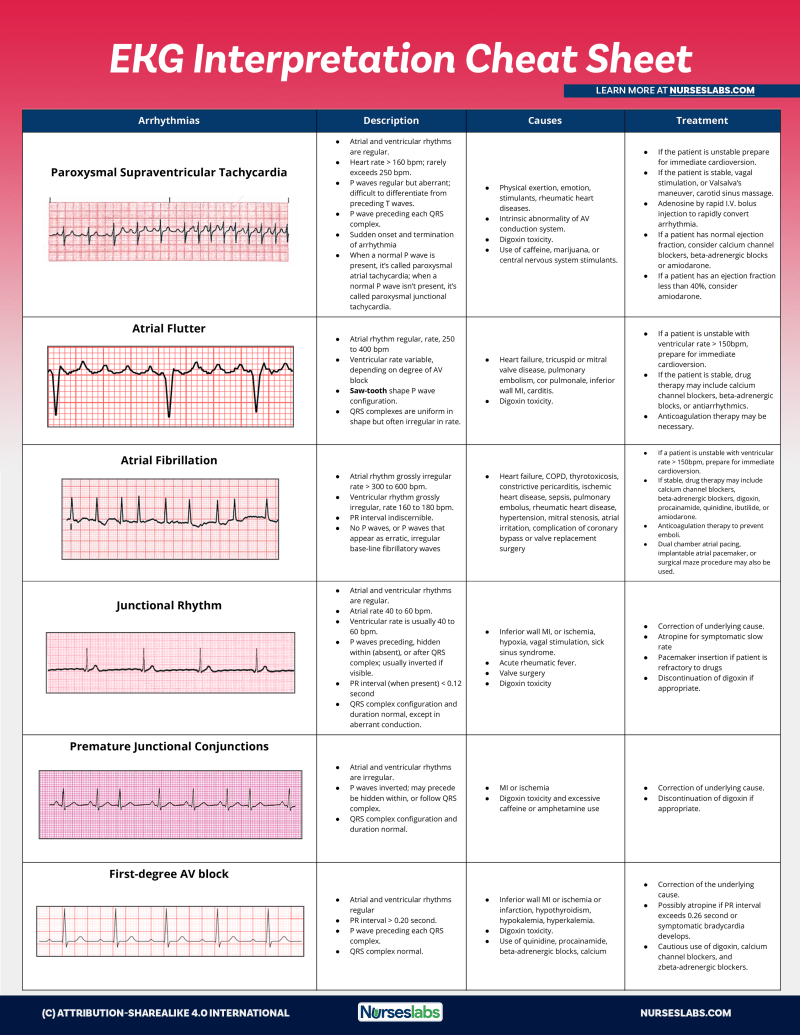
Atrial flutter is an abnormal rhythm that occurs in the atria of the heart. Atrial flutter has a regular atrial rhythm but the atrial rate is between 250 and 400 beats/min. It has a granular form. The QRS complex has a uniform shape but is often irregular in frequency.
Causes include heart failure, tricuspid or mitral valve disease, pulmonary embolism, cor pulmonale, inferior myocardial infarction, myocarditis, and digoxin toxicity.

If the patient is unstable with a ventricular rate greater than 150 bpm, prepare for immediate cardioversion. If the patient is stable, drug treatment may include calcium channel blockers, beta-adrenergic blockers, or antiarrhythmic drugs. Anticoagulants may be needed because blood stagnates in the atria.
Ecg Axis Interpretation • Litfl • Ecg Library Basics
Atrial fibrillation is random and uncoordinated twitching of the atrial muscle due to rapid generation of atrial impulses. These arrhythmias have the following symptoms:
Causes include atherosclerosis, heart failure, congenital heart disease, chronic obstructive pulmonary disease, hypothyroidism, and thyrotoxicosis. Atrial fibrillation may be asymptomatic but clinical manifestations may include palpitations, shortness of breath, and pulmonary edema. The goal of the nurse is to implement appropriate treatment to reduce ventricular response, decrease atrial excitability, and eliminate the cause.
Premature junctional contractions (PJC) occur when certain areas of the heart become more excitable than normal. It has the following characteristics.
Causes of PJC may include myocardial infarction or ischemia, digoxin toxicity, and excessive caffeine or amphetamine use. Management includes treatment of the underlying cause, discontinuing digoxin if appropriate.
The Ecg Made Easy: Hampton Dm Ma Dphil Frcp Ffpm Fesc, John, Hampton Md Ma Bm Bch Frcp, Joanna: 9780702074578: Amazon.com: Books
AV block is a conduction defect at the AV junction that impairs the conduction of impulses from the atria to the ventricular pathways. The three types are primary, secondary and tertiary.
First-degree AV block is asymptomatic and can be caused by inferior MI or ischemia, hyperkalemia, hypokalemia, digoxin toxicity, calcium channel blockers, amiodarone, and use of antiarrhythmic drugs. Management involves correcting the underlying cause. Administer atropine if the PR interval exceeds 0.26 seconds or symptomatic bradycardia develops.
Clinical manifestations include dizziness, weakness and irregular pulse. This may be due to inferior wall MI, cardiac surgery, acute rheumatic fever, or vagal stimulation. Treatment includes treatment of the underlying cause, atropine or temporary pacemaker for symptomatic bradycardia, and discontinuation of digoxin if appropriate.

Clinical manifestations are similar to Mobitz I. Causes include: severe coronary artery disease, anterior myocardial infarction, acute myocarditis, and digoxin poisoning. Treatment includes: atropine, epinephrine and dopamine for symptomatic bradycardia. Discontinue digoxin if appropriate. Install a pacemaker.
Incredibly Easy! Series#174; Ser.: Ecg Interpretation Made Incredibly Easy!… 9781582553559
Manifestations include hypotension, angina, and heart failure. This can be due to congenital abnormalities, rheumatic fever, hypoxia, MI, LEv disease, Lanegrey disease, and digoxin toxicity. Management includes atropine, epinephrine, and dopamine for bradycardia. Implantation of a pacemaker may also be considered.
Premature or premature ventricular contractions occur due to increased automaticity of ventricular myocytes. PVCs are generally not considered harmless but cause concern if more than six PVCs occur in a minute, if they occur in pairs or triangles if they have multiple foci, or if they occur on or near the T wave.
Clinical manifestations include palpitations, weakness, and dizziness, but most are asymptomatic. Management includes evaluation of the cause and treatment as indicated. Treatment is indicated if the patient has an underlying medical condition because PVCs can cause ventricular tachycardia or ventricular fibrillation. Assessment of life-threatening PVCs. Take antiarrhythmic medications as prescribed.
Ventricular tachycardia (VT) is three or more consecutive PVCs. It is considered a medical emergency because cardiac output (CO) cannot be maintained due to reduced diastolic filling (preload).
Stat 12 Lead Field Reference And Interpretation Guide
Clinical manifestations of VT include dizziness, weakness, shortness of breath, and unconsciousness. Causes include MI, aneurysm, CAD, rheumatic heart disease, mitral valve prolapse, hypokalemia, hyperkalemia and pulmonary embolism. Anxiety can also cause VT.
Management of pulseless VT: Initiate cardiopulmonary resuscitation; Follow ACLS protocol for defibrillation, intubation, and administration of epinephrine or vasopressin.
Management with VT pulse: If hemodynamically stable, follow the ACLS protocol to use amiodarone, if ineffective, start synchronized cardioversion.

The most common cause of ventricular fibrillation is myocardial ischemia or myocardial infarction. It can occur as a result of untreated ventricular tachycardia, electrolyte imbalance, digoxin or quinide toxicity, or hypothermia. Clinical manifestations may include loss of consciousness, loss of pulse, drop in blood pressure, apnea, possible seizures, and sudden death.
Lead Ecg Placement: Diagram And Mnemonic For Limb And Precordial Electrode Location — Ezmed
Download a handout to explain the EKG below. To download, click on the image below and save.
Matt Vera, a registered nurse since 2009, facilitates the learning process, breaks down complex topics, and finds creative ways to help aspiring nurses become full-time magazine writers and editors. Help students reach their full potential as providers. Provide healthcare services in the future.
Buffer Copy Email Facebook Flipboard Hacker News Line LinkedIn Messenger Mix Pinterest Pocket Print Reddit SMS Telegram Tumblr Print. For example, cardiologists often do this test to determine if the heart is healthy. They are also commonly used to test for various heart conditions.
There are several components of an EKG test that are important to reading the test strips. To begin with, each EKG is made up of a large box containing smaller boxes. Both sets of boxes measure time and distance. A large box, often called a ‘big box’ (5mm), is equivalent to 0.20 seconds. On the other hand, a small box (1 mm) shows 0.04 seconds.
How To Read An Ecg
A 12-lead ECG records a 10-second rhythm strip. On this strip, the activity of the heart is translated into drawn lines. The rise and fall of the EKG cycle are called waves that represent different phases of the heart’s activity. To read an EKG, it is important to understand the components of the waves.
The PR interval lasts from the onset of atrial depolarization (the P wave) to the onset of ventricular depolarization (QRS complex).
The QRS complex records electrical activity through the lower chambers of the heart. It represents ventricular depolarization or contraction. It also includes…

The P wave at the beginning of the ECG cycle should be present and vertical. Absent or inverted P waves are uncommon.
Buy Ekg: Ekg Interpretation Made Easy: A Complete Step By Step Guide To 12 Lead Ekg/ecg Interpretation & Arrhythmias (ekg Book, Ekg Interpretation, Nclex, Nclex Rn, Nclex Review) Online At Desertcartindia
Wave P should also be no more than 1 large square high and 1 large square wide. A typical duration is usually between 0.06 – 0.12 seconds.
The next step is to measure the PR interval. To do this, count the number of small cells between the beginning of the P wave and the peak of the QRS complex. Then, multiply that number by 0.04 seconds.
To measure the QRS complex, count the number of small boxes from the beginning to the end of the QRS complex, then divide by 0.04 seconds.
There are several methods to determine the heart rate using an EKG/ECG. Note that a normal resting range is between 60 BPM and 100 BPM per minute.
How To Read An Ekg Strip In 5 Steps
Several different methods are widely used to accurately measure the heart rate, depending on whether the rhythm is regular or irregular.
If your heart rate is regular, you can use the Big Box method. To do this, divide
12 lead made easy, barbara aehlert ecgs made easy, 12 lead ecgs, interpreting ecg made easy, ecgs made easy, ecgs made easy 6th edition, ecgs made easy aehlert, ecgs made incredibly easy, ecgs made easy 7th edition, interpreting 12 lead ecg, ecgs made easy 5th edition, reading ecgs made easy